As we navigate the aging process, we often hear mixed messages regarding health risks, particularly concerning cancer. For many, cancer risk seems to increase steadily with age, peaking during one’s 60s and 70s. However, recent research is uncovering a paradoxical phenomenon: after reaching about 80 years of age, the incidence of cancer appears to decline. This article explores groundbreaking findings that may illuminate the factors driving this intriguing trend.
The relationship between aging and cancer risk is multifaceted and deeply rooted in biological mechanisms. For years, it has been recognized that accumulating genetic mutations contribute to heightened cancer risks in older adults. Each decade of life can usher in a host of mutations, some of which may predispose individuals to various cancers. Nevertheless, researchers are beginning to explore the reasons behind a potential decrease in cancer risk among the elderly population, particularly those above 80.
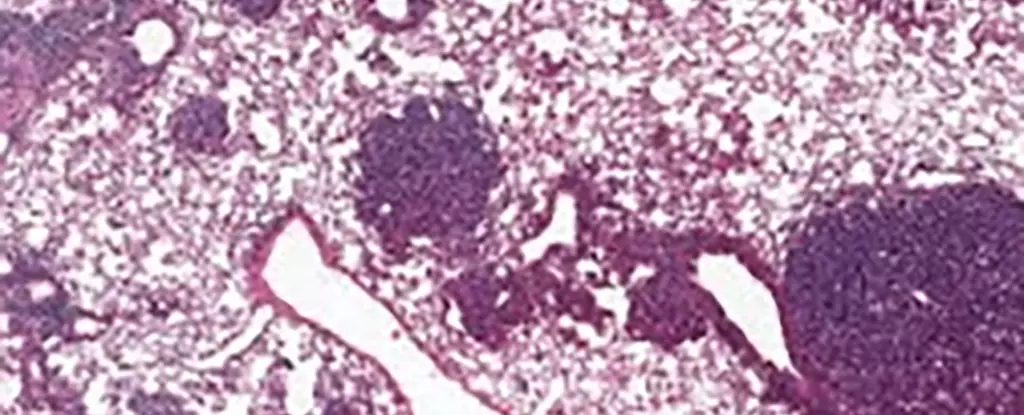
One key area of investigation involves alveolar type 2 (AT2) stem cells in the lungs. These cells play a critical role in lung regeneration and are often implicated in the development of lung cancers. Interestingly, new studies suggest that older individuals exhibit a particular change in the behavior of these cells, which may contribute to a reduction in cancerous growths as they age.
Recent international research has revealed elevated levels of a protein known as NUPR1 in older mice, a finding that has significant implications for understanding impaired lung regeneration and cancer growth. NUPR1 appears to affect how cells utilize iron—the essential mineral vital for numerous biological processes. Strikingly, despite older cells harboring more iron, they behave as if they are iron-deficient.
Dr. Xueqian Zhuang of the Memorial Sloan Kettering Cancer Center articulates the perplexity surrounding this phenomenon, stating that aging cells exhibit limited regenerative capabilities due to this paradoxical “functional iron deficiency.” This impaired capacity not only stifles normal cellular turnover but may also curb the rampant growth characteristic of cancer cells. As scientists delve deeper into this intriguing interplay, the pathway appears ripe for therapeutic exploration.
The findings from this research can open new avenues for tackling cancer, particularly through the lens of iron metabolism. By manipulating iron levels or decreasing NUPR1 expression, scientists may rejuvenate the growth potential of aging cells. Such strategies could be especially beneficial for those recovering from pulmonary issues, such as long COVID, where lung functionality is compromised.
Additionally, the relationship between NUPR1 and ferroptosis—an iron-dependent form of cell death—provides another layer of complexity in cancer therapeutics. Notably, older cells demonstrate a resistance to treatments aimed at inducing ferroptosis due to their altered iron metabolism. Therefore, the timing of these therapies may play a crucial role in their efficacy, suggesting that an earlier intervention could yield better outcomes.
This research offers critical insights into cancer prevention, particularly highlighting the need for vigilance in younger populations. Dr. Tuomas Tammela suggests that the environmental exposures we encounter during our most formative years—be it smoking or excessive sun exposure—may pose a greater carcinogenic risk than previously acknowledged. This finding underscores the necessity of proactive health measures to mitigate cancer risks from a young age.
Furthermore, the study emphasizes the importance of tailoring cancer treatments to individual circumstances, incorporating not only the cancer type and stage but also the patient’s age and overall health condition. The complexity of aging and cancer biology necessitates a more personalized approach to treatment in order to enhance outcomes and the quality of life for patients at every age.
The evolving understanding of how aging influences cancer biology uncovers a treasure trove of further questions concerning stem cell behavior, iron metabolism, and cellular regulation. As researchers continue to investigate the roles of proteins like NUPR1 and their impact on regeneration and cancer growth, the hope for more effective and individualized cancer therapies becomes increasingly tangible.
While age undoubtedly plays a significant role in cancer risk, it is crucial to appreciate the nuanced interactions of biological processes at play. The findings from these recent studies not only advance our understanding of cancer but also propose new strategies for prevention and treatment, steering us towards a future where cancer management is as personalized as it is effective.