The question of whether antibiotic use might influence the development of dementia remains an area of keen interest. As more data emerges, recent studies shed light on this complex relationship, bringing both clarity and confusion. The most recent analysis suggests that the use of antibiotics does not correlate with an increased risk of dementia in healthy older adults. Yet, the implications of these findings warrant careful consideration, particularly when evaluating their applicability to broader demographics of older adults.
The prospective study undertaken by Andrew Chan, MD, MPH, and his team at Harvard Medical School aimed to investigate the potential link between antibiotic use and dementia risk over a follow-up period of nearly 4.7 years. Focusing on a cohort of over 13,500 older adults aged 70 and above, the study relied on observational data accumulated from participants in the ASPREE trial, which was initially centered on assessing the benefits of aspirin. Upon analyzing the data, the researchers reported no significant association between antibiotic use and the incidence of dementia (Hazard Ratio [HR] 1.03) or cognitive impairment without dementia (HR 1.02).
These results seem to contradict earlier studies that had drawn correlations between antibiotic use and cognitive decline. For instance, data from the Nurses’ Health Study II indicated that women who took antibiotics for more than two months during midlife reported lower cognitive scores years later. This inconsistency reflects the intricacies inherent in studying cognitive health across different populations and methodologies.
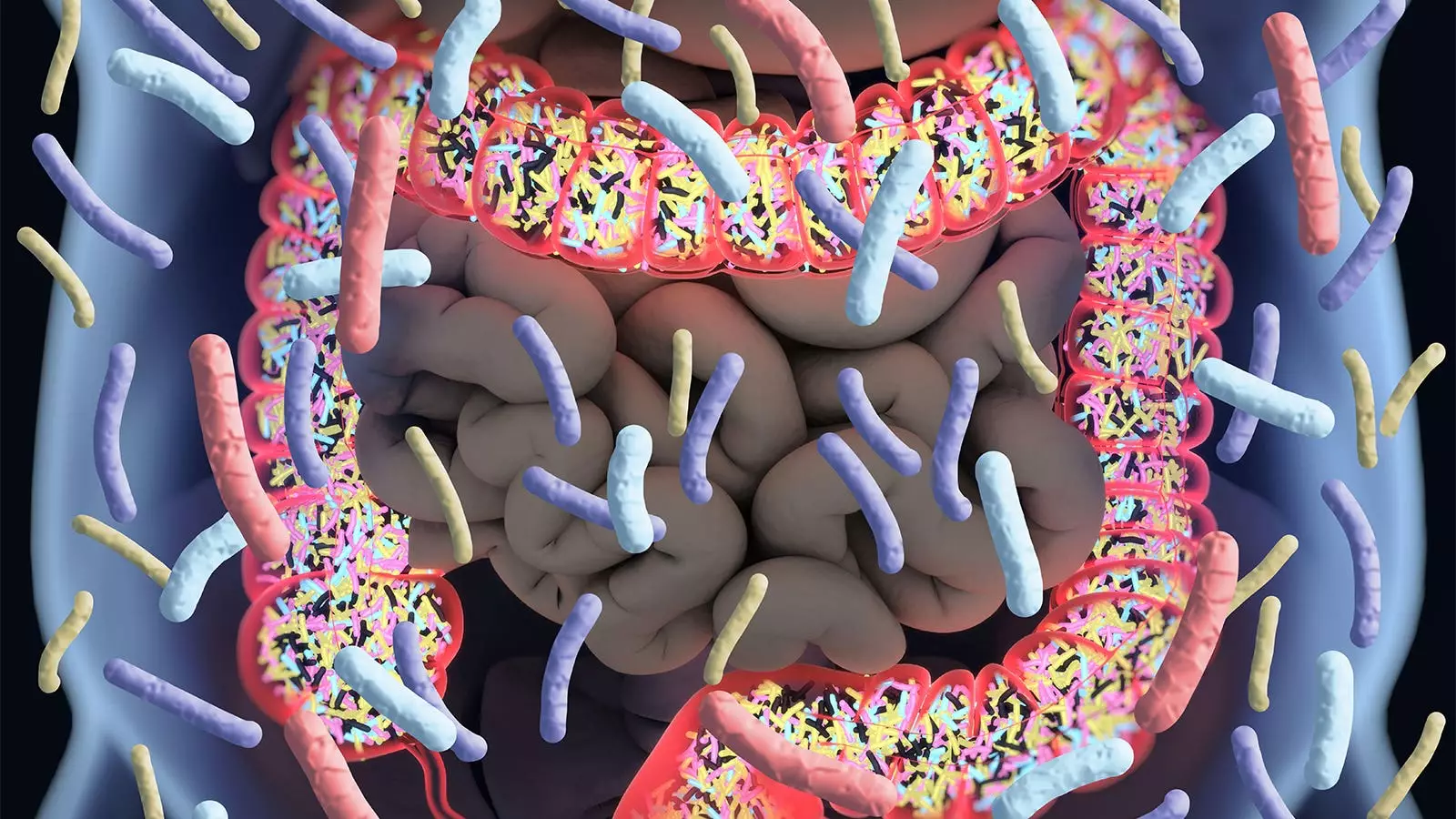
Antibiotics are known for their ability to disrupt the gut microbiome, a community of microorganisms that plays a crucial role in maintaining overall health. Chan pointed out that there have been speculations that such disruption could lead to negative consequences on cognitive function, given the microbiome’s influence on neurodegenerative processes. This concern is heightened in older adults, a demographic that frequently requires antibiotic treatment yet also faces increased risks for cognitive impairments and dementia. However, Chan, along with his co-authors, provided a measure of reassurance about the safety of antibiotics in this population based on their findings.
While the study’s outcomes offer a degree of comfort, it is essential to highlight that they come with significant caveats. The study sample primarily comprised healthy older adults, leading experts such as Wenjie Cai, MD, and Alden Gross, PhD, to urge caution regarding the generalizability of the findings. Their commentary emphasizes that while the data may inform clinical practice for those fitting the same profile as the study participants, it does not extend easily to older individuals with existing health complications or comorbidities.
Despite the valuable insights gained from Chan’s study, the research is not without limitations. For one, the reliance on filled prescription records as a measure of actual antibiotic usage poses questions about accuracy. There is a potential for discrepancies between prescribed antibiotics and actual consumption. Additionally, the ASCREE trial recruited participants who did not present with serious health issues, which raises concerns regarding the representativeness of the sample. It is unclear how these findings would translate to older adults who are already dealing with cognitive decline or other health challenges.
Such limitations necessitate a cautious approach in interpreting the results. The absence of positive correlation between antibiotic use and dementia in this particular cohort does not provide adequate grounds for dismissing concerns over the long-term effects of antibiotics on brain health in elderly populations with a more varied health status.
The findings from Chan and colleagues contribute valuable knowledge to an ongoing discourse surrounding antibiotic use and cognitive health; however, they must be viewed through a nuanced lens. While their research offers reassurance for healthy older adults regarding antibiotic prescriptions, it simultaneously highlights the necessity for further investigation to understand the potential consequences of antibiotic treatments in a broader, more diverse population. As we progress into an era of personalized medicine, understanding the intricacies of how medications affect different individuals, especially the elderly, becomes crucial. The relationship between antibiotics and cognition underscores the complexity of healthcare, where further research remains imperative to guide clinical decisions effectively.