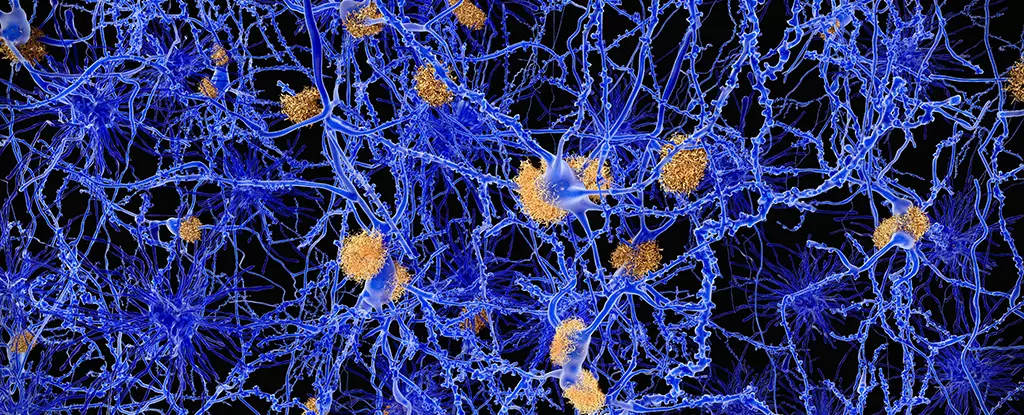
In the relentless fight against Alzheimer’s disease and other neurodegenerative disorders, the development of innovative treatments is not just desirable; it is essential. The recent breakthroughs in nanotechnology, particularly concerning the manipulation of protein structures, showcase a potential paradigm shift in how we combat these diseases. Central to this ongoing revolution are novel nanomaterials that possess the remarkable ability to combat the formation of toxic protein aggregates— a fundamental aspect of neurodegenerative diseases.
The pivotal research led by an international team, headed by materials scientist Samuel Stupp from Northwestern University, unveils a profoundly intricate relationship between specially designed nanomaterials and misfolded proteins. Traditional therapeutic approaches have often targeted the symptoms rather than addressing the core problem, which lies in the misfolding of amyloid beta proteins. The innovative use of peptide amphiphiles, compounds that exhibit hydrophilic and hydrophobic properties, presents a transformative strategy, trapping these proteins before they escalate into insidious plaques.
Understanding the Dangers of Protein Misfolding
At the heart of neurodegenerative diseases is the phenomenon of protein misfolding. When proteins like amyloid beta lose their structure, they start aggregating into fibers that penetrate neurons, causing irreversible damage. These misfolded proteins are not merely by-products of aging; they are deadly agents that impede cognitive function and erode the very essence of memory and identity. The need for an effective intervention cannot be overstated, especially given the escalating global incidence of dementia, now estimated at ten million new cases annually.
The traditional focus has often been on removing established amyloid plaques rather than preventing their formation. However, Stupp’s research flips this narrative. By employing a method that destabilizes the protein structures at an earlier stage, it opens a new frontier of preventative intervention. This “clean-up crew” approach isn’t merely a new tactic; it’s a foundational shift in how we conceptualize treatment—one that prioritizes early action over late-stage remediation.
A Closer Look at the Innovative Ingredients
Key to the success of this nanomaterial approach is the combination of peptide amphiphiles and trehalose, a naturally occurring sugar with protective properties. Trehalose has shown promise in cellular protection, helping stabilize proteins against misfolding. When integrated with the amphiphiles, trehalose alters the molecular environment, making it less rigid and more susceptible to interactions with amyloid beta. This encouraging synergy could drastically reduce the formation of toxic aggregates—a feature that’s critically needed in the field of Alzheimer’s research.
Despite these promising developments, it is vital to recognize that this research remains in its infancy. The transition from laboratory success to clinical application involves navigating a multitude of regulatory hurdles and conducting comprehensive safety and efficacy testing in human subjects. The excitement surrounding these findings should be tempered with a dose of realism, acknowledging the lengthy road ahead.
Future Implications and Ethical Considerations
As we peer into the future of Alzheimer’s treatment, the potential implications of this research extend beyond merely mitigating symptoms. If successful, this strategy could redefine our therapeutic landscape, offering individuals at risk of neurodegenerative diseases a fighting chance against the debilitating march of cognitive decline. However, it also raises fundamental ethical questions about accessibility and the urgency of developing treatments before it’s too late.
For too long, pharmaceutical advancements have paralleled socio-economic divides, where life-saving treatments become a privilege rather than a right. As governments and biomedical companies funnel resources into this transformative research, they must also consider how to ensure equitable access to these groundbreaking treatments once they achieve regulatory approval. The promise of such nanotechnology cannot be allowed to become another casualty of pharmaceutical inequity.
The integration of nanotechnology into neurodegenerative disease treatment initiatives isn’t just about science; it’s about crafting a future where Alzheimer’s, once a near-certain descent into loss, is met with renewed hope and resilience. Embracing these advancements could very well lead us towards a society that not only fights against but ultimately prevails in the battle against neurodegeneration.